Navigating Cervical Cancer: A Comprehensive Guide for Women
Cervical cancer is a preventable and treatable condition when detected early. Understanding its causes, symptoms, and prevention can help women protect their health and save lives.
For more wellness and health awareness content, visit our Health Blog.
What Is Cervical Cancer?
Cervical cancer is a type of cancer in women that begins in the cells of the cervix, the lower, narrow end of the uterus (womb).
The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time.
Before cancer fully develops, cervical cells may go through precancerous changes, also known as cervical dysplasia, in which abnormal cells appear in the cervical tissue.
If not detected and treated, these abnormal cells can progress into cancer cells, which may grow deeper into the cervix and spread to surrounding tissues.
The cervix has two main parts:
- Ectocervix (exocervix): The outer part of the cervix visible during a gynecologic exam. The ectocervix is covered with thin, flat squamous cells.
- Endocervix: The inner canal of the cervix that connects the vagina to the uterus. The endocervix is lined with column-shaped glandular cells that produce cervical mucus.
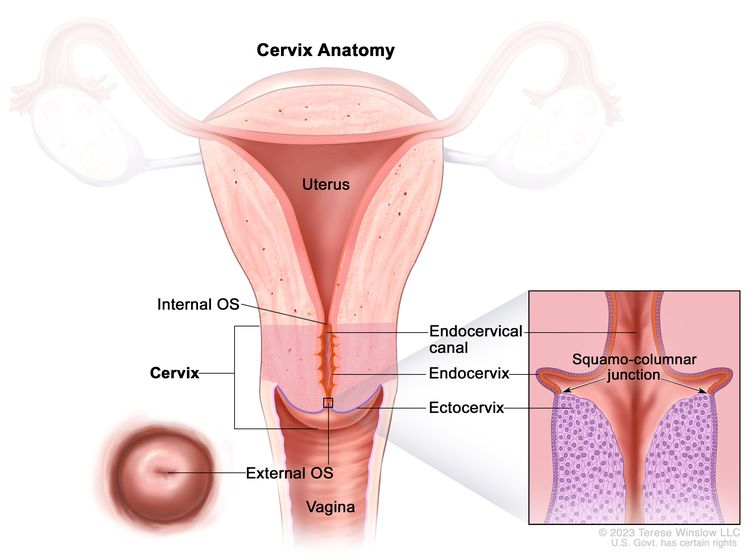
The cervix is the lower, narrow end of the uterus that connects the uterus to the vagina. It consists of several important parts:
- Internal OS: The opening between the cervix and the upper part of the uterus.
- Endocervix: The inner portion of the cervix, forming the endocervical canal, is lined with glandular cells that produce mucus.
- Ectocervix: The outer part of the cervix that projects into the vagina and is covered with squamous cells, which are thin, flat cells.
- External OS: The opening between the cervix and the vagina.
The junction where the endocervix and ectocervix meet is called the squamocolumnar junction, also known as the transformation zone.
This area contains both glandular cells from the endocervix and squamous cells from the ectocervix, and it is a critical site where most cervical cancers originate.
Understanding the Different Types of Cervical Cancer:
Main Types of Cervical Cancer
- Squamous Cell Carcinoma (SCC)
- Adenocarcinoma
- Adenosquamous Carcinoma (Mixed Carcinoma)
- Characteristics: Contains both squamous and glandular cancer cells.
- Prevalence: Represents about 3–10% of cervical cancer cases.
- Treatment: Managed similarly to squamous cell carcinoma.
- Characteristics: Contains both squamous and glandular cancer cells.
Rare Subtypes of Cervical Cancer
- Small Cell Neuroendocrine Carcinoma
- Prevalence: Scarce, accounting for less than 5% of cervical cancers.
- Behavior: Highly aggressive and tends to spread quickly.
- Clear Cell Adenocarcinoma
- Association: Often linked to in utero exposure to diethylstilbestrol (DES).
- Prevalence: Scarce.
- Association: Often linked to in utero exposure to diethylstilbestrol (DES).
- Glass Cell Carcinoma
- Sarcoma and Lymphoma
- Prevalence: Scarce; these are non-epithelial cancers that can occur in the cervix.
Early and Advanced Symptoms of Cervical Cancer Every Woman Should Know:
Cervical cancer often develops slowly and may not show symptoms in the early stages. Early detection through regular Pap smear and HPV screening is critical.
When symptoms do appear, they may include:
Common Symptoms
- Abnormal vaginal bleeding: Bleeding between periods, after sexual intercourse, or post-menopause.
- Unusual vaginal discharge: May be watery, bloody, or have a foul odor.
- Pelvic pain: Pain during sexual intercourse or persistent pelvic discomfort.
- Painful urination: Discomfort or burning sensation while urinating.
Advanced Symptoms
- Leg swelling or pelvic swelling due to cancer spread.
- Unexplained weight loss or fatigue.
- Back pain or pain in the lower abdomen.
- Loss of bladder or bowel control in severe cases.
What Causes Cervical Cancer?
Cervical cancer develops when abnormal cells in the cervix grow uncontrollably.
The primary causes and risk factors include:
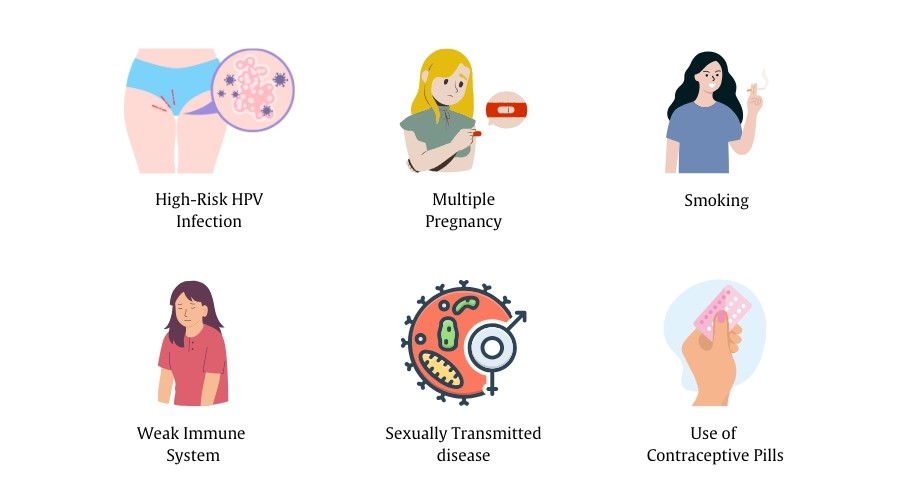
1. Human Papillomavirus (HPV) Infection
- HPV is the most significant cause of cervical cancer.
- High-risk HPV types, especially HPV 16 and HPV 18, can lead to cervical dysplasia and eventually cancer.
- HPV is usually transmitted through sexual contact.
2. Multiple Sexual Partners and Early Sexual Activity
- Having multiple sexual partners or becoming sexually active at a young age increases the risk of HPV infection, which in turn raises the risk of cervical cancer.
3. Weakened Immune System
- Conditions that suppress immunity, such as HIV/AIDS or long-term immunosuppressive therapy, increase susceptibility to persistent HPV infection.
4. Smoking
- Tobacco use contributes to cervical cell abnormalities and increases the risk of developing cervical cancer.
5. Long-term Use of Oral Contraceptives
- Studies suggest extended use of birth control pills may slightly increase cervical cancer risk, especially in women with HPV infection.
6. Other Risk Factors
- Family history of cervical cancer.
- Previous cervical cancer or precancerous lesions.
- Exposure to diethylstilbestrol (DES) in utero.
Cervical Cancer Screening and Diagnosis:
Family history of cervical cancer, previous precancerous lesions, or DES exposure.
Chronic conditions like high blood pressure and diabetes may also weaken the immune system, making it harder for the body to fight HPV infections.
1. Pap Smear (Pap Test)
- Detects abnormal cervical cells before they turn into cancer.
- Recommended for women aged 21–65 regularly.
- Early detection through a Pap smear significantly reduces cervical cancer risk.
2. HPV Testing
- Identifies infection with high-risk human papillomavirus (HPV) types like HPV 16 and 18.
- Often combined with a Pap smear (co-testing) for accurate results.
3. Colposcopy
- A detailed examination of the cervix using a colposcope.
- Performed if the Pap smear or HPV test shows abnormal results.
- Allows biopsy of suspicious areas for histopathological analysis.
4. Cervical Biopsy
- Confirms the presence of cancerous or precancerous cells.
- Types include punch biopsy, cone biopsy, and endocervical curettage.
5. Imaging Tests
- Advanced cervical cancer may require a CT scan, an MRI, or a PET scan to determine cancer spread.
Cervical Cancer Prevention Guide: Vaccination, Pap Smear, and Screening Strategies
Cervical cancer is largely preventable through two primary approaches: HPV vaccination and regular screening. These strategies are endorsed by global health authorities like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC).
1. HPV Vaccination
Human Papillomavirus (HPV) is the leading cause of cervical cancer. Vaccination against HPV is a highly effective preventive measure.
- Recommended Age: The CDC and the American Cancer Society recommend HPV vaccination for preteens aged 11–12 years, but it can be administered starting at age 9. Vaccination is also advised for individuals up to age 26 who have not been previously vaccinated.
- Vaccine Schedule: For those starting the vaccination series before age 15, a two-dose schedule is recommended, with doses given 6 to 12 months apart. Individuals starting the series at age 15 or older should receive a three-dose schedule.
- Effectiveness: The HPV vaccine is most effective when administered before exposure to the virus, offering protection against the HPV types most commonly associated with cervical cancer.
2. Regular Screening
Early detection through screening can identify precancerous changes in the cervix, allowing for timely intervention.
- Pap Smear (Pap Test): Recommended every 3 years for women aged 21–29. For women aged 30–65, screening every 5 years with a combination of Pap test and HPV testing is advised.
- HPV Testing: For women aged 30–65, primary HPV testing every 5 years is an alternative to the Pap test.
- Self-Sampling: Emerging guidelines suggest that women aged 30–65 may opt for self-collected HPV tests every 5 years, which can increase screening accessibility.
3. WHO Global Strategy
The WHO has set ambitious targets to eliminate cervical cancer as a public health problem by 2030:
- 90% of girls are fully vaccinated with the HPV vaccine by age 15.
- 70% of women screened using a high-performance test by age 35 and again by age 45.
- 90% of women with precancerous lesions were treated, and 90% of women with invasive cancer were managed.
4. Additional Preventive Measures
- Avoid Smoking: Tobacco use increases the risk of cervical cancer in women with HPV infection.
- Safe Sexual Practices: Reducing the number of sexual partners and using barrier methods can lower the risk of HPV infection.
- Regular Health Check-ups: Routine gynecological exams can help detect abnormalities early. For more insights on general wellness, read
- 👉 Everything You Need to Know About Leatheling: A Comprehensive Guide to Its Uses, Benefits, and Future Trends.
Prognosis and Survival Rates of Cervical Cancer
The prognosis of cervical cancer depends largely on the stage at diagnosis, overall health, and response to treatment.
Early detection through Pap smear and HPV testing significantly improves survival outcomes.
Survival Rates by Stage
- Stage I (cancer confined to the cervix):
- 5-year survival rate: Approximately 90–95%
- 5-year survival rate: Approximately 90–95%
- Stage II (cancer has spread beyond the cervix but not to the pelvic wall):
- 5-year survival rate: Around 70–80%
- 5-year survival rate: Around 70–80%
- Stage III (cancer extends to the pelvic wall or lower vagina):
- 5-year survival rate: About 40–50%
- Stage IV (cancer has spread to distant organs):
- 5-year survival rate: Approximately 15–20%
Factors Affecting Prognosis
- Early detection through regular cervical cancer screening
- Type of cervical cancer (squamous cell carcinoma vs adenocarcinoma)
- Patient age and overall health
- Treatment options: Surgery, chemotherapy, radiotherapy, or combination therapy.
FAQ’s:
1. What is cervical cancer?
Cervical cancer originates in the cervix—the lower part of the uterus connecting to the vagina. It often develops from persistent high-risk HPV infections, leading to abnormal cell changes known as cervical dysplasia.
2. What are the early symptoms of cervical cancer?
Early-stage cervical cancer may not present noticeable symptoms. As the disease progresses, common signs include:
- Abnormal vaginal bleeding (e.g., after intercourse, between periods, or post-menopause)
- Unusual vaginal discharge (watery, bloody, or foul-smelling)
- Pelvic pain or pain during intercourse
- Painful urination or blood in urine
3. What causes cervical cancer?
- Persistent HPV infection, smoking, weakened immunity, and chronic illnesses like diabetes can increase the risk.
4. How is cervical cancer diagnosed?
Diagnosis involves:
- Pap smear (to detect abnormal cells)
- HPV testing (to identify high-risk strains)
- Colposcopy (magnified examination of the cervix)
- Cervical biopsy (to confirm cancerous cells)
- Imaging tests (e.g., CT, MRI, PET scans) to determine cancer spread.
5. Can cervical cancer be prevented?
Yes, prevention strategies include:
- HPV vaccination (recommended for girls and boys aged 9–14)
- Regular cervical cancer screening (Pap smear and HPV testing)
- Safe sexual practices (e.g., using condoms)
- Avoiding smoking
Conclusion:
Cervical cancer is one of the most preventable forms of cancer in women.
Key takeaways for prevention and early detection:
- HPV vaccination prevents up to 70% of cases.
- Regular screening raises early survival rates to 90–95%.
- Healthy habits and early check-ups save lives.
To learn more about overall health, prevention, and wellness topics, visit our
👉 Health Blog and explore related insights on
👉 Cancer Awareness.

Pingback: Best Healthy Diet Plans for Weight Management: Weight Loss & Weight Gain Guide - leatheling