Diabetes: Causes, Symptoms, Treatment, and Prevention Guide

What Is Diabetes?
Diabetes is a chronic health condition where blood sugar (glucose) levels stay too high. This happens when the pancreas doesn’t make enough insulin or when the body cannot use insulin properly — a condition known as insulin resistance.
Insulin acts like a “key” that helps glucose from food enter your cells for energy. When insulin isn’t working properly, glucose builds up in the bloodstream, leading to high blood sugar (hyperglycemia).
Over time, uncontrolled diabetes can cause serious health problems, including heart disease, kidney damage, nerve damage, and vision loss. high blood pressure management.
Diabetes can affect children, adults, and seniors, but it is manageable through healthy lifestyle changes, diabetes medication, and blood sugar monitoring.
Types of Diabetes:
Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose).
There are several types of diabetes, but the most common are Type 1 diabetes, Type 2 diabetes, Prediabetes, and Gestational diabetes.
Knowing these types helps in early diagnosis, diabetes management, and prevention.
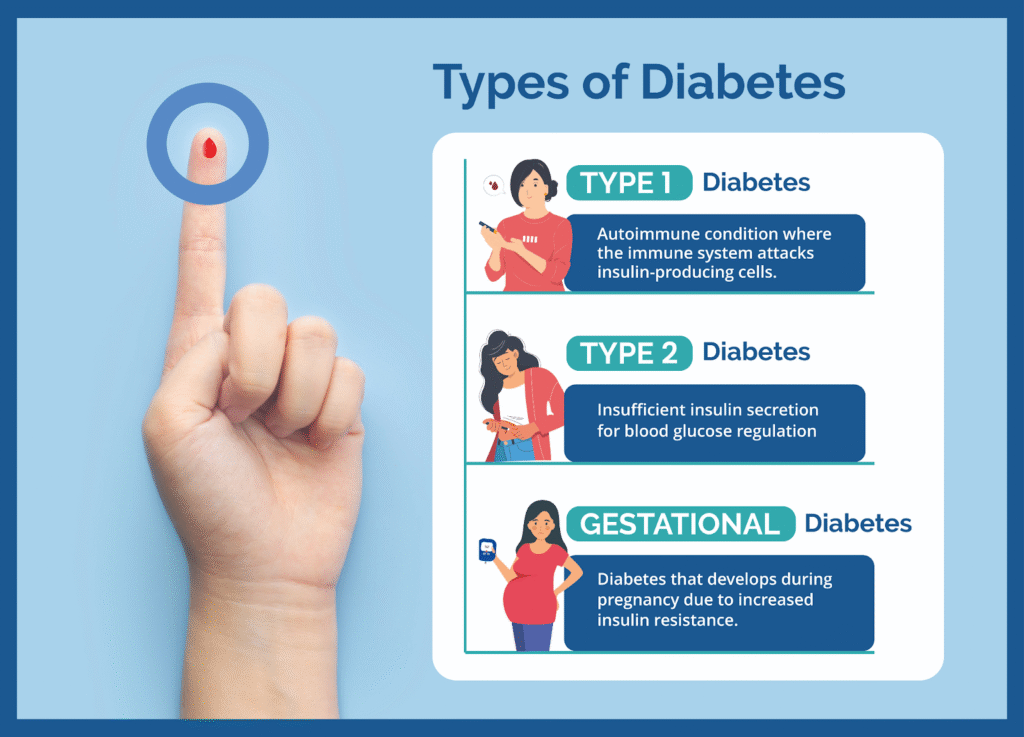
Type 1 Diabetes:
Type 1 diabetes is an autoimmune disease where the immune system attacks the pancreas, stopping it from making insulin.
- Accounts for 5–10% of diabetes cases.
- Requires daily insulin therapy to control blood sugar levels.
- Usually diagnosed in children and young adults, but it can develop at any age.
- Common symptoms: frequent urination, extreme thirst, fatigue, and sudden weight loss.
- Keywords used: type 1 diabetes, autoimmune diabetes, insulin therapy, high blood sugar symptoms.
Type 2 Diabetes:
Type 2 diabetes is the most common form of diabetes, affecting 90–95% of patients worldwide.
- Caused by insulin resistance (body cells don’t respond to insulin) and reduced insulin production.
- Strongly linked to obesity, unhealthy diet, lack of exercise, and genetics.
- Managed through healthy eating, weight loss, physical activity, oral diabetes medication, or insulin.
- Keywords used: type 2 diabetes, insulin resistance, diabetes treatment, diabetes management, high blood sugar.
Gestational Diabetes;
Gestational diabetes occurs during pregnancy due to hormonal changes affecting insulin function.
- Usually diagnosed between 24–28 weeks of pregnancy.
- Increases the risk of complications for both mother and baby.
- Raises the chances of developing Type 2 diabetes later in life.
- Managed with a healthy diet, exercise, and blood sugar monitoring.
- Keywords used: gestational diabetes, pregnancy diabetes, blood sugar in pregnancy, pregnancy health.
Prediabetes:
Prediabetes is the warning stage before Type 2 diabetes, where blood glucose levels are higher than normal but not high enough for a diabetes diagnosis.
- Affects 1 in 3 adults, but most don’t know they have it.
- Lifestyle changes like a healthy diet, exercise, and weight loss can prevent diabetes progression.
- Keywords used: prediabetes, high blood sugar, prevent type 2 diabetes, diabetes risk factors.
How Common Is Diabetes?
Diabetes is very common worldwide and continues to rise each year. In the United States, about 37.3 million people (around 11% of the population) are living with diabetes.
Among these cases, Type 2 diabetes is the most common, making up 90–95% of all diabetes cases.
Globally, an estimated 537 million adults have diabetes. Experts predict this number will increase to 643 million by 2030 and reach 783 million by 2045, highlighting the growing need for diabetes awareness, prevention, and treatment.
What Causes Diabetes?
The causes of diabetes vary depending on the type, but they all lead to high blood sugar (hyperglycemia) due to problems with insulin production or insulin resistance.
Causes of Type 1 Diabetes:
- Autoimmune reaction – the immune system attacks and destroys pancreatic beta cells that make insulin.
- Genetic factors – family history increases risk.
- Environmental triggers – certain viruses may trigger the immune system response.
- Keywords: type 1 diabetes causes, autoimmune diabetes, pancreatic insulin destruction.
Causes of Type 2 Diabetes:
- Insulin resistance – cells stop responding to insulin properly.
- Genetics – family history and ethnicity play a big role.
- Obesity and poor diet – high-calorie, sugary diets increase risk.
- Physical inactivity – lack of exercise worsens insulin sensitivity.
- Age factor – risk increases after age 45, though younger people are increasingly affected.
- Keywords: type 2 diabetes causes, insulin resistance, obesity, lifestyle risk factors.
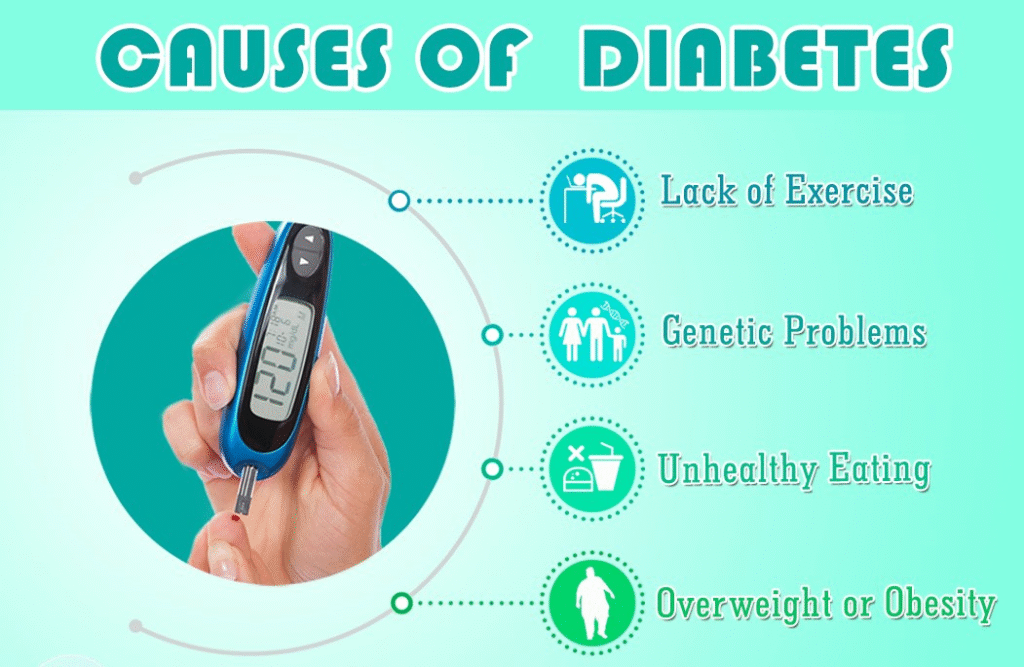
Causes of Gestational Diabetes:
- Hormonal changes during pregnancy make cells resistant to insulin.
- Family history of type 2 diabetes or gestational diabetes.
- Overweight or obesity before pregnancy.
- Keywords: gestational diabetes causes, pregnancy hormones, blood sugar in pregnancy.
Other Possible Causes:
- Pancreatic diseases (pancreatitis, pancreatic cancer).
- Hormonal disorders (Cushing’s syndrome, PCOS).
- Certain medications (steroids, antipsychotics) that raise blood sugar levels.
- Genetic mutations leading to rare forms like MODY or neonatal diabetes.
Symptoms of Diabetes
Recognizing the symptoms of diabetes early is essential for timely diagnosis and treatment.
Common signs of high blood sugar (hyperglycemia) include:
- Increased thirst (polydipsia) and dry mouth
- Frequent urination (especially at night)
- Extreme fatigue or lack of energy
- Blurred vision or sudden vision changes
- Unexplained weight loss despite eating normally
- Numbness or tingling in hands or feet (nerve damage)
- Slow-healing wounds, sores, or cuts
- Frequent skin infections or vaginal yeast infections
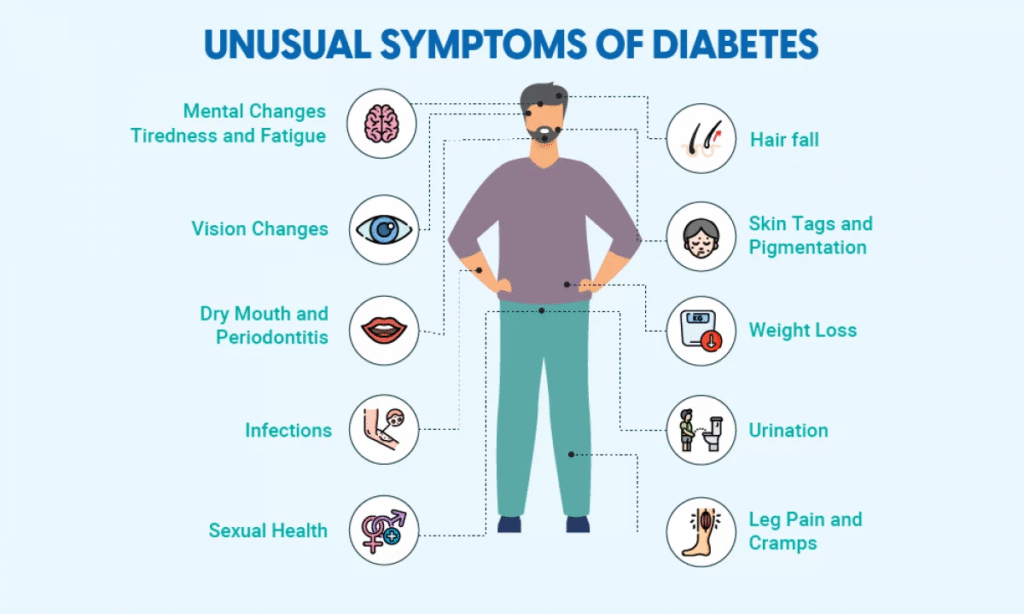
Symptoms by Type of Diabetes
Type 1 Diabetes Symptoms:
- Develop quickly — often within weeks or months.
- May include symptoms of diabetes-related ketoacidosis (DKA), a serious complication.
- DKA warning signs: vomiting, stomach pain, fruity-smelling breath, and labored breathing (medical emergency).
Type 2 Diabetes & Prediabetes Symptoms:
- Often mild or unnoticeable in the early stages.
- Many people are diagnosed only after routine blood tests show high blood sugar.
- Prediabetes sign: darkened skin patches on the neck, armpits, or groin (acanthosis nigricans).
Gestational Diabetes Symptoms:
- Usually has no noticeable symptoms.
- Detected through screening tests between 24–28 weeks of pregnancy.
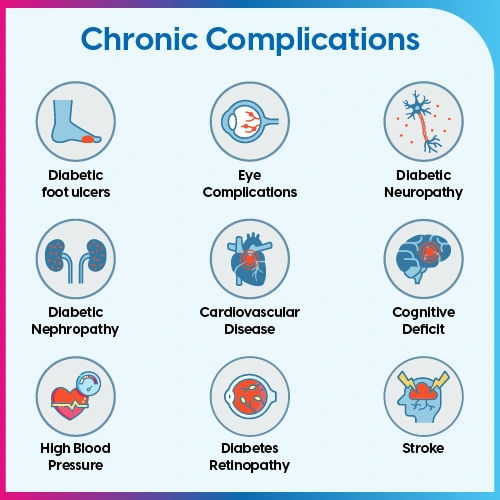
Complications of Diabetes
Uncontrolled diabetes can lead to both acute (sudden) and chronic (long-term) complications, primarily caused by prolonged high blood sugar (hyperglycemia) or severe fluctuations in glucose levels.
Recognizing these complications early can prevent life-threatening outcomes.
Acute Complications of Diabetes:
Acute complications occur suddenly and require immediate medical attention:
- Hyperosmolar Hyperglycemic State (HHS):
- More common in Type 2 diabetes.
- Occurs when blood sugar exceeds 600 mg/dL for a prolonged period, leading to severe dehydration, confusion, and possible coma.
- Emergency treatment is necessary.
- More common in Type 2 diabetes.
- Diabetes-Related Ketoacidosis (DKA):
- Mostly affects people with Type 1 diabetes or undiagnosed diabetes.
- Happens when there’s not enough insulin, forcing the body to break down fat for energy, producing ketones that make blood acidic.
- Symptoms: vomiting, abdominal pain, fruity breath odor, labored breathing, and unconsciousness.
- Requires urgent hospitalization.
- Mostly affects people with Type 1 diabetes or undiagnosed diabetes.
- Severe Hypoglycemia (Low Blood Sugar):
- Occurs when blood sugar drops dangerously low.
- Common in people using insulin therapy.
- Symptoms: blurred or double vision, clumsiness, confusion, seizures.
- Requires immediate treatment with glucagon or medical intervention.
- Occurs when blood sugar drops dangerously low.
Long-Term Complications of Diabetes
Chronic high blood sugar can damage blood vessels, nerves, and organs, leading to severe health issues:
Cardiovascular Complications (Most Common)
- Coronary Artery Disease
- Heart Attack
- Stroke
- Atherosclerosis (hardening of arteries) high blood pressure management
Nerve & Organ Damage
- Neuropathy: Numbness, tingling, or pain in hands and feet.
- Nephropathy: Kidney damage leading to kidney failure or need for dialysis/transplant.
- Retinopathy: Eye damage that may lead to vision loss or blindness.
- Gastroparesis: Slowed stomach emptying causes nausea and digestive problems.
Other Long-Term Issues
- Diabetic Foot Ulcers and risk of amputation.
- Skin infections and slow-healing wounds.
- Hearing loss.
- Sexual dysfunction (erectile dysfunction, vaginal dryness).
- Gum disease and oral health problems.
Mental Health Complications:
People with diabetes are 2–3 times more likely to experience depression or anxiety, making mental health management an important part of diabetes care.
How Is Diabetes Diagnosed? Tests & Procedures Explained
Diabetes diagnosis is based on measuring blood sugar (glucose) levels using specific medical tests.
Early and accurate diagnosis is crucial to preventing diabetes complications and starting proper treatment.
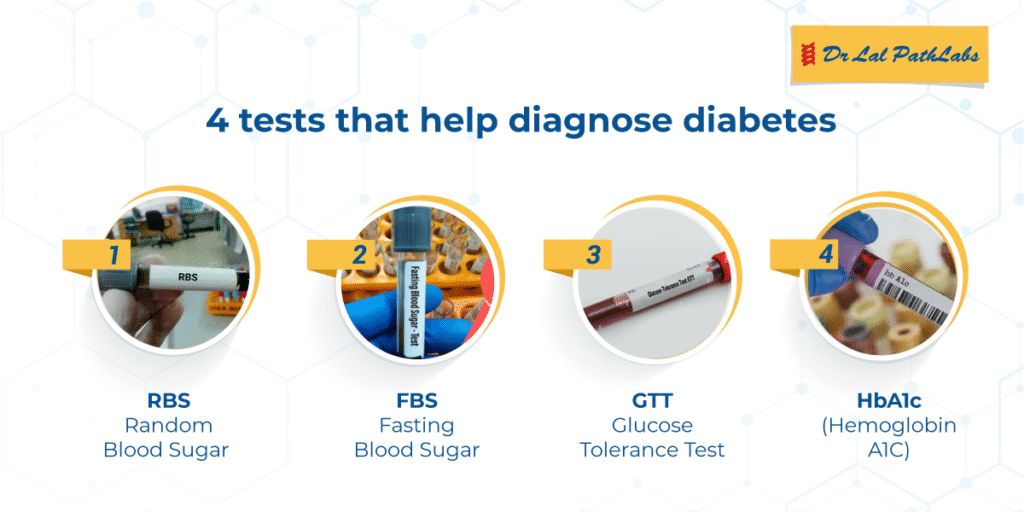
Common Diagnostic Tests for Diabetes
Fasting Blood Sugar (FBS) Test:
- Measures blood sugar after at least 8 hours of fasting.
- Results:
- Normal: <100 mg/dL
- Prediabetes: 100–125 mg/dL
- Diabetes: ≥126 mg/dL (confirmed on repeat test)
- Normal: <100 mg/dL
HbA1c Test (Glycated Hemoglobin Test):
- Shows average blood sugar levels over the past 2–3 months.
- Results:
- Normal: Below 5.7%
- Prediabetes: 5.7% – 6.4%
- Diabetes: 6.5% or higher
Oral Glucose Tolerance Test (OGTT):
- Measures blood sugar before and after drinking a glucose solution.
- Results after 2 hours:
- Normal: <140 mg/dL
- Prediabetes: 140–199 mg/dL
- Diabetes: ≥200 mg/dL
- Normal: <140 mg/dL
Random Blood Sugar Test:
- Can be done anytime during the day, regardless of meals.
- Diabetes is diagnosed if the level is ≥200 mg/dL with symptoms like excessive thirst, urination, or fatigue.
Gestational Diabetes Screening (During Pregnancy)
- Typically performed between 24–28 weeks of pregnancy using the OGTT to detect gestational diabetes.
Why Early Diagnosis Matters?
Timely diagnosis helps:
- Start lifestyle changes and medications early.
- Prevent or delay diabetes complications like heart disease, kidney damage, and neuropathy.
- Improve long-term health outcomes and quality of life.
Diabetes Management and Treatment: Effective Ways to Control Blood Sugar
Managing diabetes is all about keeping your blood sugar levels within a healthy range to prevent complications and improve your quality of life.
Treatment depends on the type of diabetes (Type 1, Type 2, or gestational diabetes) but usually involves a combination of lifestyle changes, medications, and regular monitoring.
1. Lifestyle Modifications
Healthy habits are the first line of diabetes management:
- Balanced Diet:
- Focus on whole grains, vegetables, lean protein, and healthy fats.
- Limit sugary foods, processed snacks, and refined carbs.
- Use the plate method to control portions.
- Focus on whole grains, vegetables, lean protein, and healthy fats.
- Regular Exercise:
- At least 150 minutes of activity weekly — walking, swimming, or cycling. Improves insulin sensitivity and supports high blood pressure management.
- Weight Management:
- Even a 5–10% weight loss can significantly improve blood sugar control, especially for Type 2 diabetes.
- Even a 5–10% weight loss can significantly improve blood sugar control, especially for Type 2 diabetes.
- Quit Smoking & Limit Alcohol:
- Smoking increases the risk of diabetes complications (heart disease, stroke).
- Drink alcohol in moderation to avoid blood sugar spikes.
- Smoking increases the risk of diabetes complications (heart disease, stroke).
2. Medications for Diabetes Treatment
- Oral Medications (Type 2 Diabetes):
- Metformin is usually the first-line medication.
- Other classes include SGLT2 inhibitors, GLP-1 receptor agonists, and DPP-4 inhibitors.
- Metformin is usually the first-line medication.
- Insulin Therapy (Type 1 & Severe Type 2):
- Necessary for people whose bodies don’t make enough insulin.
- Delivered via injections or insulin pumps.
- Necessary for people whose bodies don’t make enough insulin.

3. Blood Sugar Monitoring
- Use a glucometer or continuous glucose monitor (CGM) to track your blood sugar daily.
- Helps adjust diet, activity, and medication doses in real-time
4. Stress Management
- Chronic stress can raise blood sugar levels.
- Practice yoga, meditation, or deep breathing exercises.
Diabetes Prevention: Proven Ways to Lower Your Risk
While Type 1 diabetes cannot be prevented, Type 2 diabetes and prediabetes can often be delayed or avoided with simple lifestyle changes.
Preventing diabetes means keeping your blood sugar levels, weight, and overall health in check.

1. Maintain a Healthy Weight
- Even a 5–10% weight loss can significantly reduce the risk of developing Type 2 diabetes.
- Focus on gradual, sustainable weight loss through a balanced diet and regular exercise.
2. Eat a Balanced, Low-Sugar Diet
- Choose whole grains, vegetables, fruits, lean proteins, and healthy fats.
- Limit sugary drinks, refined carbs, and processed foods that spike blood sugar.
- Include fiber-rich foods to improve insulin sensitivity.
3. Stay Physically Active
- Aim for 30 minutes of moderate exercise most days (walking, cycling, swimming).
- Physical activity helps regulate blood sugar levels and improves metabolism.
4. Avoid Smoking and Limit Alcohol
- Smoking increases the risk of insulin resistance and heart disease.
- Keep alcohol consumption moderate to avoid blood sugar spikes.
5. Get Regular Screenings
- Routine blood sugar testing can catch prediabetes early.
- Early detection allows for quick lifestyle interventions and prevents progression to diabetes.
6. Manage Stress
- Chronic stress can increase cortisol levels, leading to higher blood sugar.
- Practice meditation, yoga, or breathing exercises to stay mentally healthy.
When to See Your Healthcare Provider for Diabetes?
Knowing when to see a doctor for diabetes is essential for early diagnosis and effective diabetes management.
If You Haven’t Been Diagnosed with Diabetes:
Schedule a visit with your healthcare provider if you notice common diabetes symptoms, such as:
- Increased thirst (polydipsia)
- Frequent urination
- Fatigue
- Unexplained weight loss
- Blurred vision
Early blood sugar testing can help detect prediabetes or Type 2 diabetes before complications develop.
If You Have Diabetes:
If you’ve already been diagnosed, regular check-ups are crucial:
- See your endocrinologist or primary care doctor for routine diabetes monitoring.
- Get HbA1c tests as recommended (usually every 3–6 months).
- Discuss any new symptoms like numbness, vision changes, or slow-healing wounds immediately.
Living with Diabetes: Support and Care
Being diagnosed with diabetes can feel overwhelming, but with the right diabetes care plan, you can live a happy and healthy life.
- Stay consistent: Monitor your blood sugar, take medications, and follow your meal plan.
- Build a support system: Work with your doctor, diabetes educator, and include family members in your care.
- Ask for help: Don’t hesitate to contact your healthcare provider if you face challenges in controlling your blood sugar.
FAQ’s:
What is diabetes?
Diabetes is a chronic condition where your blood sugar (glucose) levels stay too high due to insufficient insulin production or the body’s inability to use insulin properly.
What are the early symptoms of diabetes?
Common early signs of diabetes include:
- Increased thirst and frequent urination
- Fatigue
- Blurred vision
- Unexplained weight loss
- Slow-healing wounds
If you notice these symptoms, see your doctor for a blood sugar test.
What causes diabetes?
The causes of diabetes vary by type:
- Type 1 Diabetes: Autoimmune attack on insulin-producing cells.
- Type 2 Diabetes: Insulin resistance and poor lifestyle habits.
- Gestational Diabetes: Hormonal changes during pregnancy
How is diabetes diagnosed?
Doctors use tests such as:
- Fasting Blood Sugar (FBS)
- HbA1c Test
- Oral Glucose Tolerance Test (OGTT)
These measure your blood glucose levels to confirm a diagnosis.
Can diabetes be cured?
There’s no cure for diabetes, but it can be managed effectively through:
- Healthy diet and exercise
- Medications or insulin therapy
- Regular blood sugar monitoring
How can I prevent diabetes?
You can reduce your risk of Type 2 diabetes by:
- Maintaining a healthy weight
- Eating a balanced, low-sugar diet
- Exercising regularly
- Avoiding smoking and limiting alcohol
Conclusion:
Diabetes is a common but manageable condition. Whether you are dealing with Type 1 diabetes, Type 2 diabetes, prediabetes, or gestational diabetes, the key to living well is early diagnosis, proper treatment, and consistent lifestyle changes.
By monitoring blood sugar levels, following a balanced diet, exercising regularly, taking prescribed medications or insulin, and staying in touch with your healthcare provider, you can prevent serious diabetes complications such as heart disease, kidney damage, and vision loss.
Remember, diabetes management is a lifelong journey, but with the right knowledge and support, you can lead a healthy, active, and fulfilling life.

Pingback: Kentucky Counselling Center: Services, Online Therapy & How to Get Help - leatheling
Pingback: Do You Need a Passport to Go to Hawaii? Your Easy Guide - LeatHeling